Diagnosing plasminogen deficiency type 1 (PLGD-1)

Plasminogen activity test
Confirm a suspected case of PLGD-1 with a simple blood test for plasminogen activity, CPT® code: 85420, available in many major US labs with results in under 5 days.1-3*

Clinical evaluation
Each patient with plasminogen deficiency type 1 can present in a unique manner, with symptoms varying from person to person.
It is vital to run a thorough evaluation, assessing for signs of both internal and external lesions, as PLGD-1 is a systemic disease and internal lesions can occur without clinical suspicion.3

Family medical history
Since PLGD-1 is an autosomal recessive disorder,* testing a patient's family members, particularly siblings, can help identify undiagnosed cases. Symptoms may vary widely even among members of the same family.3
It is vital to coordinate care with a hematologist for comprehensive evaluation and treatment of internal lesions.3
*Plasminogen activity reference ranges vary by lab. Be sure to review results carefully. In adults, the average normal range is 70-130%. Because activity levels don't always reflect symptom severity, patients with levels near the lower limit of normal should still be evaluated closely.2,4,5
Supporting a PLGD-1 diagnosis
An antigen test indicating decreased levels of plasminogen in the blood can support a PLGD-1 diagnosis, but cannot confirm it on its own.1
Lesion biopsy showing fibrin-rich deposits in the biopsied tissue can support a PLGD-1 diagnosis, but cannot confirm it on its own.1,6*
*Lesion removal prior to diagnosis is not recommended3
Genetic testing revealing a mutation in the gene coding for plasminogen can confirm a PLGD-1 diagnosis and screen asymptomatic family members, but is not required to diagnose.1†
†An activity test is typically needed to ensure treatment coverage
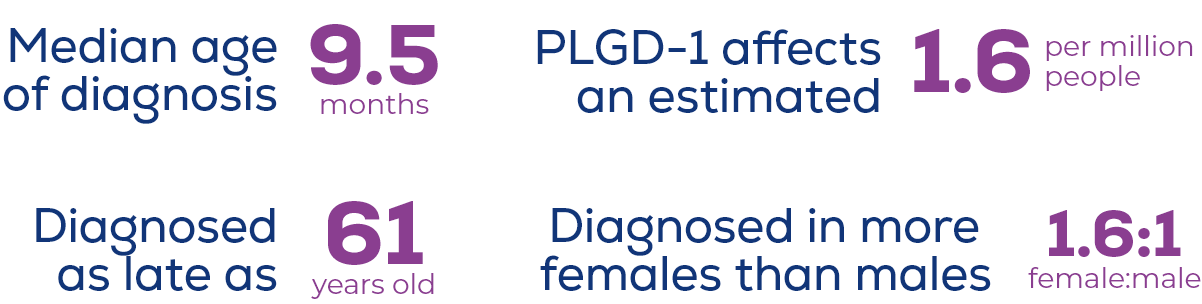
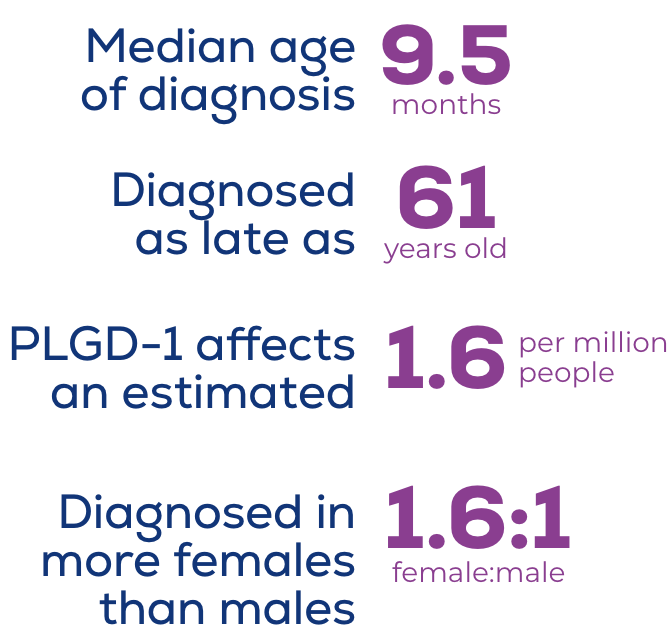
Initial diagnosis of PLGD-1 can occur at any age6-8
PLGD-1 is rare with highly variable symptoms that resemble more common conditions and can fluctuate over time, leading to missed or delayed diagnoses.3 An estimated 1.6 per million people are affected by PLGD-1.6 While it is an autosomal recessive disorder, PLGD-1 is diagnosed more frequently in females than males for reasons not yet understood.9
Accurate documentation supports patient access and reimbursement
Review the billing and coding guide for the most up-to-date ICD-10 and CPT coding information.
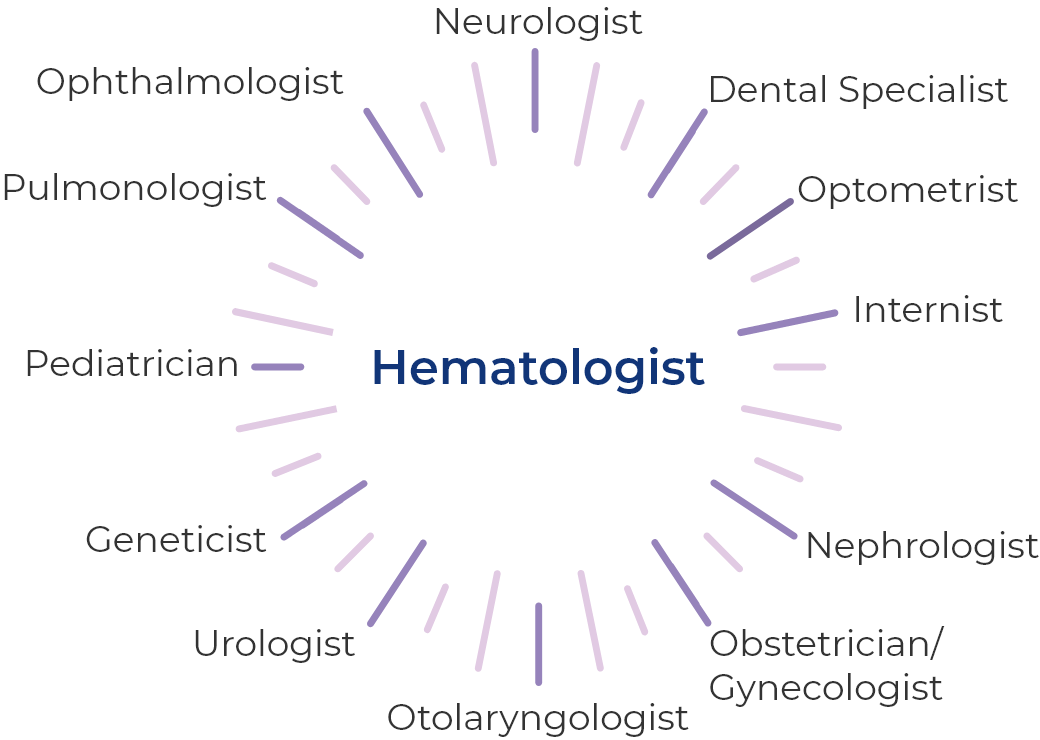
Managing PLGD-1 often requires multidisciplinary coordination with a hematologist at the center3
An array of specialists can serve as initial points of care and often help with ongoing management of PLGD-1 depending on the patient's case, age, and lesion location.10
Coordinate with a hematologist
INDICATIONS AND USAGE
RYPLAZIM® (plasminogen, human-tvmh) is a plasma-derived human plasminogen indicated for the treatment of patients with plasminogen deficiency type 1 (hypoplasminogenemia).
IMPORTANT SAFETY INFORMATION
CONTRAINDICATIONS:
RYPLAZIM is contraindicated in patients with known hypersensitivity to plasminogen or other components of RYPLAZIM.
WARNINGS AND PRECAUTIONS:
- Bleeding: RYPLAZIM administration may lead to bleeding at active mucosal disease-related lesion sites or worsen active bleeding not related to disease lesions. Discontinue RYPLAZIM if serious bleeding occurs. Monitor patients during and for 4 hours after infusion when administering RYPLAZIM to patients with bleeding diatheses and patients taking anticoagulants, antiplatelet drugs, or other agents which may interfere with normal coagulation.
- Tissue Sloughing: Respiratory distress due to tissue sloughing may occur in patients with mucosal lesions in the tracheobronchial tree following RYPLAZIM administration. Please monitor appropriately.
- Transmission of Infectious Agents: RYPLAZIM is made from human plasma and therefore carries a risk of transmitting infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent, and theoretically, the Creutzfeldt-Jakob Disease (CJD) agent.
- Hypersensitivity Reactions: Hypersensitivity reactions, including anaphylaxis, may occur with RYPLAZIM. If symptoms occur, discontinue RYPLAZIM and administer appropriate treatment.
- Neutralizing Antibodies: Neutralizing antibodies (inhibitors) may develop, although they were not observed in clinical trials. If clinical efficacy is not maintained (e.g., development of new or recurrent lesions), determine plasminogen activity trough levels in plasma.
- Laboratory Abnormalities: Patients receiving RYPLAZIM may have elevated blood levels of D-dimer. D-dimer levels will lack interpretability in patients being screened for venous thromboembolism (VTE).
ADVERSE REACTIONS:
The most frequent (incidence ≥ 10%) adverse reactions in clinical trials were abdominal pain, bloating, nausea, fatigue, extremity pain, hemorrhage, constipation, dry mouth, headache, dizziness, arthralgia, and back pain.
To report SUSPECTED ADVERSE REACTIONS, contact KEDRION at 1-855-427-6378 or the FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Click here for the RYPLAZIM Full Prescribing Information.
This site is intended for residents of the US only.
References:
1. Mehta R, Shapiro AD. Plasminogen deficiency. Haemophilia. 2008;14(6):1261-1268. 2. Plasminogen activity. Machaon Diagnostics. Accessed December 11, 2025. https://www.machaondiagnostics.com/test/plasminogen-activity 3. Shapiro AD, Nakar C. How I treat type 1 plasminogen deficiency. Blood. 2025;145(25):2954-2965. 4. Shapiro AD, Menegatti M, Palla R, et al. An international registry of patients with plasminogen deficiency (HISTORY). Haematologica. 2020;105(3):554-561. 5. Plasminogen activity. Quest Diagnostics. Accessed December 11, 2025. https://testdirectory.questdiagnostics.com/test/test-detail/4458/plasminogen-activity?cc=MASTER 6. Schuster V, Seregard S. Ligneous conjunctivitis. Surv Ophthalmol. 2003;48(4):369-388. 7. Schuster V, Hügle B, Tefs K. Plasminogen deficiency. J Thromb Haemost. 2007;5(12):2315-2322. 8. Klammt J, Kobelt L, Aktas D, et al. Identification of three novel plasminogen (PLG) gene mutations in a series of 23 patients with low PLG activity. Thromb Haemost. 2011;105(3):454-460. 9. Tefs K, Gueorguieva M, Klammt J, et al. Molecular and clinical spectrum of type I plasminogen deficiency: a series of 50 patients. Blood. 2006;108(9):3021-3026. 10. Congenital type 1 plasminogen deficiency. NORD. Updated Februrary 6, 2025. Accessed December 11, 2025. https://rarediseases.org/rare-diseases/congenital-plasminogen-deficiency

